1. Overproduction
Overproduction occurs when more items are produced than the subsequent step in the process requires. Materials and supplies are consumed without contributing value to the final product.

In clinical laboratories, overproduction can occur when manually preparing reagents, calibrators, or controls. Excess unused reagents are discarded, resulting in significant material waste. Additionally, manual reagent preparation makes inefficient use of staff resources, test processing workflows are disrupted, and the risk of operator errors is increased.
Testing platforms that utilize ready-to-use multiplex reagents with barcodes can eliminate manual reagent handling processes and enable lean automation. Laboratories can minimize waste caused by overproduction, optimize staff utilization, and enhance testing workflows.
2. Waiting
Waiting refers to any time lapsed without adding value to the final product.

In clinical laboratories, inefficient processes can extend testing wait times. Waiting to begin processing patient samples slows the workflow and increases turnaround time. Inefficiency can arise from batched testing, which limits throughput and further delays turnaround time. Processing multi-test panels with multiple different test methods or analyzers can also significantly delay test results.
Analyzers with continuous loading capabilities promote lean efficiencies by allowing laboratories to minimize waiting times. This allows technologists to load patient samples onto the analyzers and process tests continuously. Additionally, laboratories can capitalize on multiplex technology to reduce waiting times and enhance efficiency. Multiplexing can be used to complete multi-test panels and test algorithms with a single test. By eliminating single-analyte testing, result throughput is increased and waiting times are substantially reduced.
3. Transportation
Transportation waste occurs when materials are moved unnecessarily without adding value.
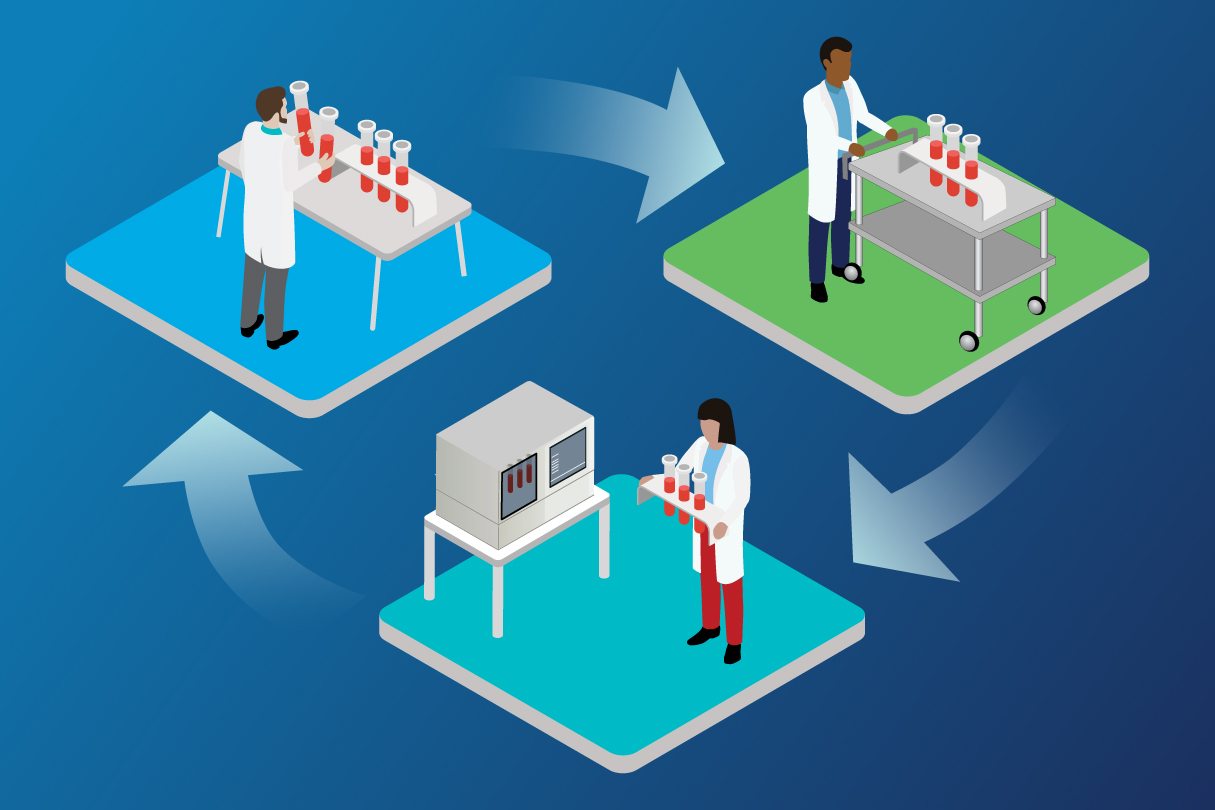
Transporting specimens between multiple test platforms is a major source of inefficiency in clinical laboratories. Moreover, inefficiencies may occur when labs employ multiple test methods and analyzers with limited test menus, small on-board test capacities, and inadequate automation capabilities that force technicians to perform manual batch testing.
Labs can improve lean processes by consolidating multiple test methods and analyzers onto a single platform. This can help minimize specimen transportation while saving laboratory space. Labs can further reduce the inefficient movement of patient samples and testing components by using automated analyzers with extensive test menus and large onboard test capacities. This can further reduce waste and optimize testing efficiency.
4. Overprocessing
Overprocessing refers broadly to waste from non-value-added work.

In clinical laboratories, overprocessing occurs when laboratory technologists perform processes that could otherwise be automated. For example, inefficient test methods may require pre-analytical sample preparation. Inefficient test methods also often necessitate further management of reflex testing algorithms, requiring technologists to perform additional patient sample handling and processing of individual add-on tests.
Primary sample tube processing enables laboratories to reduce overprocessing and improve workflow efficiency. Eliminating pre-analytical preparation steps allows samples to be processed directly from primary tubes. Additionally, to enhance management of add-on testing, labs can employ multiplex technology to complete testing algorithms without patient redraw or additional sample processing.
5. Inventory
Inventory waste occurs when resources are overstocked or stored inefficiently, adding to storage costs without adding value.

Refrigerated storage space is inherently limited in clinical laboratories. Many inefficient test methods require bulky test reagents and consumable supplies, which takes up valuable storage space. Additionally, multiple reagents are often required to perform tests that generate a single result.
Laboratories can optimize inventory storage by replacing single-analyte reagents with compact, multiplex reagent packs. These packs include the reagents needed to perform multiple tests simultaneously, all while occupying significantly less space. Laboratories can consolidate their refrigerated storage space, avoid inventory waste, and produce more test results with fewer reagents and consumable supplies.
6. Motion
Motion waste results from excess or overly complicated movements. Unlike transportation waste, which refers to the inefficient movement of testing components, motion waste involves the inefficient movement of personnel.
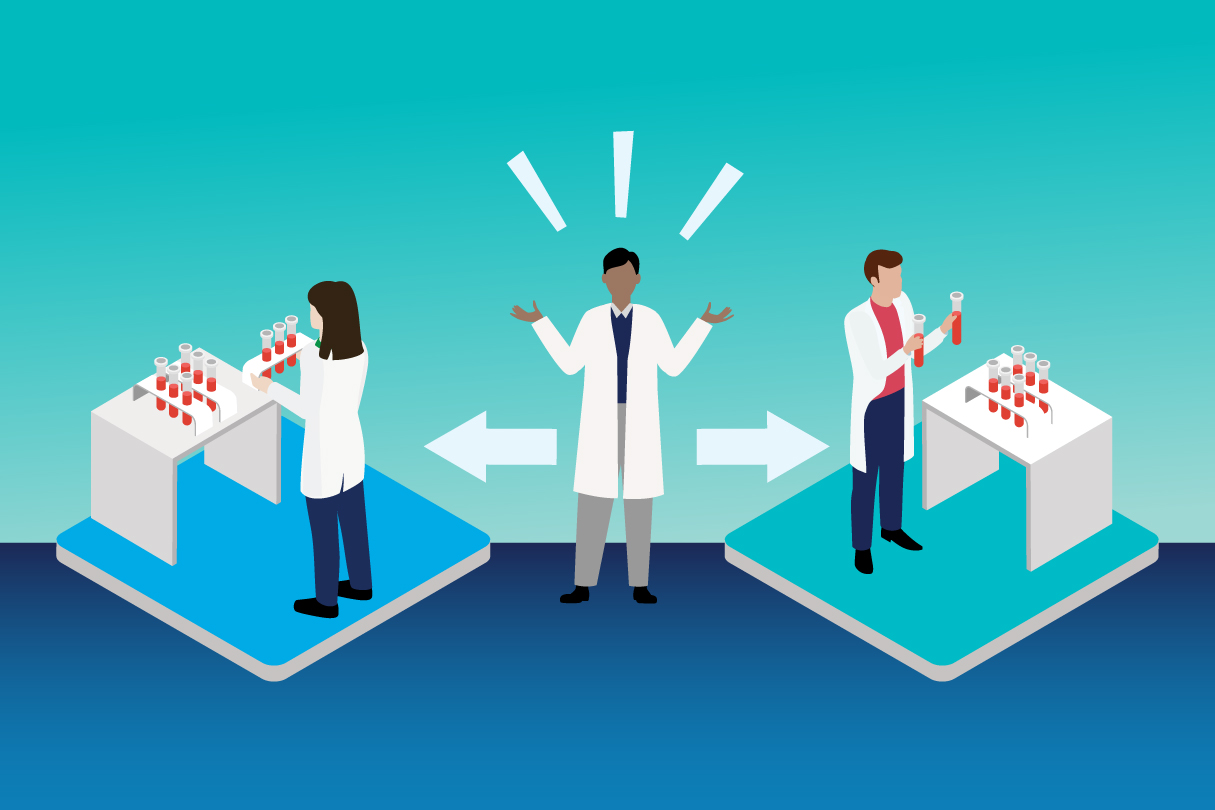
In clinical laboratories, motion inefficiencies arise from test methods that require manual processing steps, extensive maintenance, or specialized training on the part of lab technicians. Test panels may require multiple individual tests, and management of reflex testing algorithms may require technologists to perform additional tests and even redraw patient samples. Sample handling, reagent preparation, and data entry are additional common sources of excess motion.
There are several ways to minimize excess motion in the laboratory. Automation extends walkaway times while reducing manual processes and data entry that are often time-consuming and prone to error. Additionally, multiplex technology can significantly improve management of test panels and reflex testing algorithms, helping further minimize excess or inefficient motion.
7. Testing Failures
Testing failures are a form of defective work, one of the 7 wastes identified by lean principles. Like other forms of defective work, testing failures can lead to significant rework.

When tests fail in the clinical laboratory, repeat testing is required. Repeat testing is often performed in large batches, increasing reagent and labor costs and exacerbating workflow inefficiencies. This, in turn, delays or compromises results and negatively affects patient care. Additionally, many inefficient test methods rely on traditional quality control (QC) processes performed every 24 hours to detect testing failures. These QC processes may not detect errors until many patient tests have already been processed.
Labs can increase efficiency by utilizing test methods that integrate QC into every test. Integrated QC monitors assay performance and integrity of results, allowing labs to identify potential testing problems immediately and between QC runs. This helps labs minimize test failures and mitigate the risk of rework or scrap.
Conclusion
By adopting lean lab practices, clinical laboratories can minimize the 7 wastes of lean across a spectrum of methods and applications. Laboratories can:
-
Avoid overproduction with ready-to-use multiplex reagents
Reduce waiting times with continuous sample loading
Minimize transportation of specimens between multiple testing platforms by consolidating test methods
Mitigate overprocessing with primary sample tube processing
-
Increase storage capacity and avoid inventory waste with multiplex reagent packs
Eliminate wasteful lab technologist motion with automation and multiplex technologies
Reduce the risk of testing failures and repeat testing with integrated QC technology
In these ways and more, clinical laboratories can implement lean processes to enhance their operations, optimize testing throughput and turnaround time, and ultimately help improve patient care.
References
- Kanban Software for Agile Project Management (2023). 7 Wastes of Lean: How to Optimize Resources. https://kanbanize.com/lean-management/value-waste/7-wastes-of-lean, accessed September 12, 2023.
- Bharsakade R. et al. (2021). A Lean Approach to Healthcare Management Using Multi Criteria Decision Making. OPSEARCH 58(3), 610–35.




